Once the thin-section images are acquired, volume reconstruction software aids planning in difficult oral surgery procedures, allowing practitioners to straighten skewed mandibles and maxillae on the computer, getting the bite right before the surgeon lays a hand on the patient.
Not that everything has changed. Clay modeling, photography, and radiography are still the norm in most practices, and the nascent CT software market has yet to produce the perfect reconstruction application. Still, prospects seem to be improving each year as more vendors get involved, according to Dr. Jon Bradrick (DDS), who spoke last month at the American Association of Oral and Maxillofacial Surgeons (AAOMS) meeting in San Francisco.
The oral and maxillofacial surgeon shared his decades of experience in facial imaging and procedure planning with CT, dramatized with a cache of jaw-dropping case studies. Bradrick is an associate professor and director of oral and maxillofacial surgery at MetroHealth Medical Center in Cleveland, and has worked with CT since the modality's earliest days.
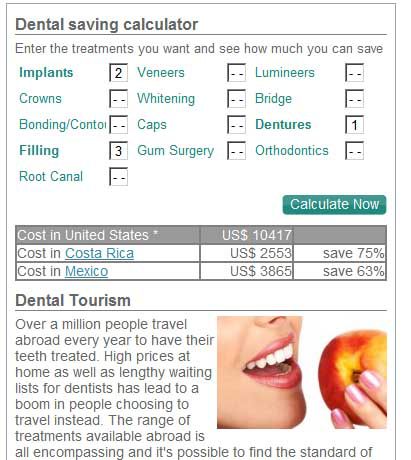
 |
| Compared to the rough, grainy images CT offered in its infancy (left), today's multislice scanners and thin-section protocols provide far more detail for maxillofacial procedure planning. All images courtesy of Dr. Jon Bradrick. |
Acquisition
Today's multislice scanners allow for planning of intricate procedures in the most difficult cases, Bradrick said. The best results start with multislice scanners, thin-collimation scanning, and zero gantry tilt. Bradrick's group uses an MX8000 scanner (
Phillips Medical Solutions, Andover, MA), "souped up" to be a 40-slice machine, he said.
"Here's a little trick I learned," Bradrick said. "If you think you're going to be doing some ... extreme CT reconstructions, I'll show you how to separate the patient's mandible and maxilla so you can manipulate them. Put a radiolucent object between the teeth, like a tongue blade or a piece of gauze that doesn't have a radiopaque marker in it, and just separate the teeth. That helps you when you try to segment out the mandible."
And don't administer contrast material unless you're looking for CT angiography results, he said. Prominent blood vessels can impede visualization of bone and cartilage.
When ordering the scan, be sure to specify anatomic landmarks for the radiologist -- from the supraorbital rims to the larynx, for example. Doing so helps radiologists "give me what I want, not what they think they want to give me," Bradrick said. "It has decreased our number of repeat scans."
Reconstruction software
Two major kinds of reconstruction software are in common use: applications coupled with CT scanners, such as the Philips Brilliance package, or software from standalone developers, such as Vworks 4.0 Clinic 3D by
CyberMed of Seoul, Korea. Both applications were used to create the images in this article.
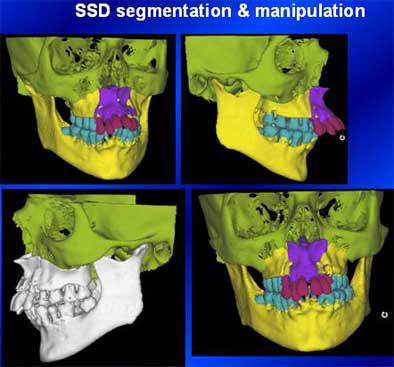
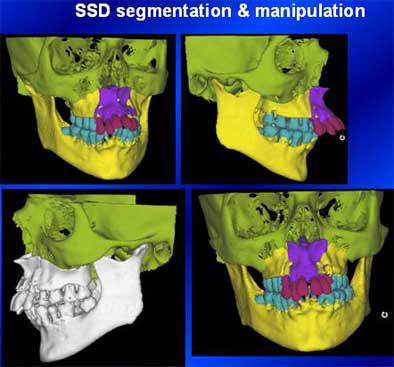
There are also two major types of reconstruction software available: traditional surface-shaded display (SSD) applications, and the newer 3D volume reconstruction products that offer complete 3D segmentation and manipulation. Reconstruction software allows the practitioner to take the CT image apart and work with it, he said, "so you can move a mandible, move a maxilla."
Both software types allow traditional 2D viewing of axial slices. Both produce minimum and maximum intensity projections, multiplanar reconstructions, and curved reconstructions, which are useful for producing dental panorexes. Both enable measurement and annotation of the anatomy for procedure planning.
However, SSD reconstruction programs get by on only about 10% of the image data, a throwback to the days of more primitive computers, Bradrick said. Offering only external topographic reconstructions, these applications apply thresholding to create a complete image from only a small portion of the CT data, resulting in poorer resolution, and more artifacts and false surfaces compared to volume 3D reconstructions, he said. And unfortunately, SSD reconstructions are the only format vendors currently use to produce stereolithographic, or 3D-printed, anatomic models.
In contrast, 3D volume reconstruction programs use 100% of the CT dataset, yielding superior image quality and the ability to depict tiny structures and fractures far better than SSD programs. The newer applications are also capable of displaying precise attenuation values and anatomic measurements, and can also produce minimum and maximum intensity projections (MIPs).
"Not a lot of people are using (volume reconstruction software)," Bradrick said. "We started using it a lot and other people started when they saw the results we were getting.... However, SSD, even with its antiquities, does do one thing for us that the newer volume reconstruction (programs) don't: segmentation and manipulation," he said.
These processes are essential to virtual surgery in the CT environment, Bradrick said. Considering the need, volume reconstruction programs that add segmentation and manipulation are certain to appear on the market eventually, Bradrick said.
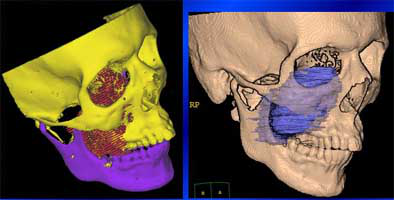
 |
| Postsurgical CT reconstruction. Image is of a young man who had suffered a serious motorcycle accident, presenting with multiple midface, frontal sinus, and frontal bone fractures. A pneumocephalus complication postsurgery required further intervention. |
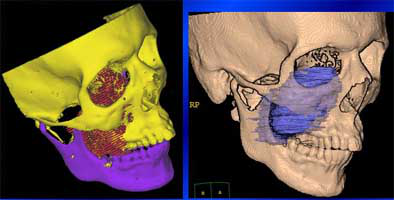 |
| Above and below: Preteen boy presenting with facial swelling had maxillary and skull base chondrosarcoma. Presurgical planning with CT reconstructions enabled precise characterization of the lesion. At three months, surgery appears to have been successful. |
 |
Orthognathic surgery
An improper bite can give rise to a host of problems related to chewing, speech, and general oral health. The standard remedy, orthodontics, simply isn't enough when the jaw needs repositioning. Orthognathic surgery can be used to reposition the mandible, maxilla, and dentoalveolar segments to achieve facial balance and correct occlusal discrepancies.
MDCT with 3D reconstruction can replace -- and improve on -- a wide range of traditional surgical planning tools such as cephalometric and panorex radiography, dental impressions, and traditional model surgery, Bradrick said. With the aid of 3D software, malocclusions and deformities of the jaw can be segmented and realigned before the patient heads to the OR.
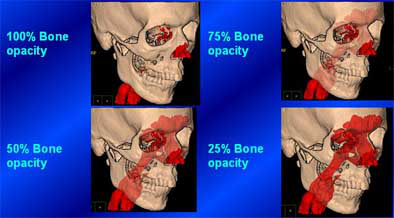
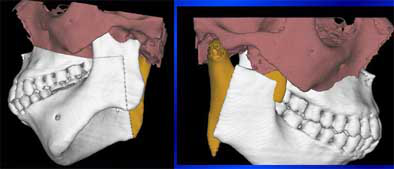 |
| Above and below: 17-year-old girl with vertical maxillary excess, maxillary and mandibular asymmetry, and a hypoplastic condyle. Multiplanar maxillary-mandibular segmentation technique with SSD 3D reconstruction was used for presurgical planning. Anterior nasal spine, left malar prominence, and finally the left mandibular condyle were tested as trial pivot points to produce the best result with the least amount of surgery. Mandibular asymmetry had re-emerged 19 months postsurgery, however. Currently 3D CT reconstructions are being compared to isolate the cause of the relapse. |
 |
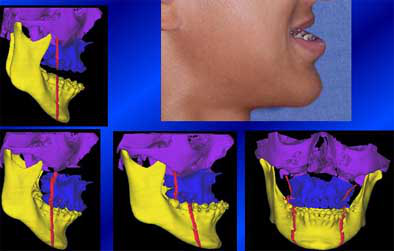
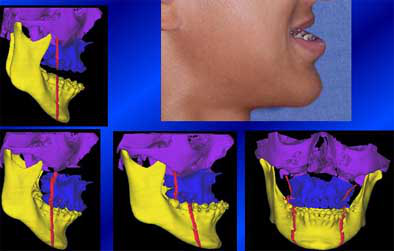
Another patient recently presented with vertical maxillary excess, mandibular hypoplasia, labial dental protrusion, and severe periodontitis, Bradrick said. She wanted dentures, "but you can't even make dentures with this (protrusion) in the middle," he said. Volumetric CT images were acquired to plan a multipiece maxillary osteotomy.
"We did all this (planning) in virtual space," Bradrick said. We select a pivot point and axis of rotation, spin the (maxilla) back, then select a point of rotation in the condyle region, and ... fix it so there's no vertical excess anymore, measure it and do the osteotomy, and see if you end up where you want to be." The teeth were taken out last and replaced with dentures.
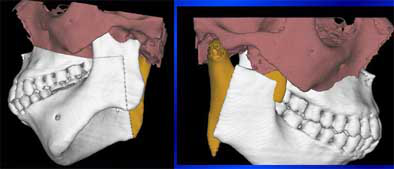
 |
 |
| Above and below: Patient with vertical maxillary excess, mandibular hypoplasia, labial dental protrusion, and severe periodontitis underwent presurgical planning with CT volume reconstructions. Anterior segmental osteotomy was used to retract the maxilla by 10 mm. Then the teeth were removed, allowing the patient to have new dentures fitted. |
 |
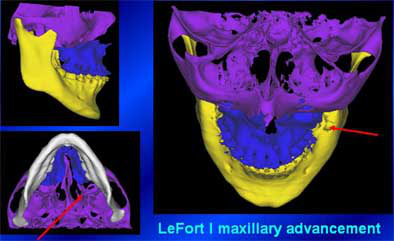
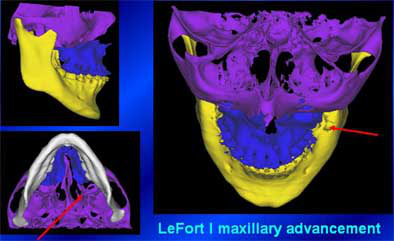
Maxillary advancement
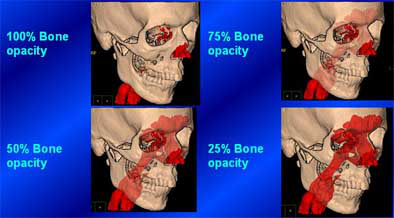
Maxillary advancement surgery is an important tool for normalizing facial contours and correcting dental occlusions. CT with volumetric reconstruction can replace the extensive photographic and modeling analysis used to plan bone-grafting techniques used to advance, retract, or tilt the maxilla in surgery. Horizontal osteotomy genioplasty, meticulously planned with CT reconstructions, can give the chin a more normal appearance than is possible with traditional alloplastic implants.
 |
| Markers (red) can be added to CT reconstructions to plan the adjustments in maxillary advancement surgery, replacing plaster modeling. Segmentation can also be performed with vectors and planes, which are especially helpful in planning genioplasty. The surgeon can move and manipulate the planes until the result is right. |
 |
Dental implants
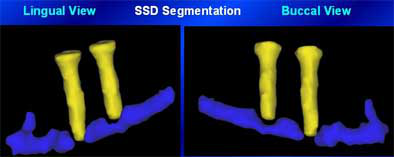
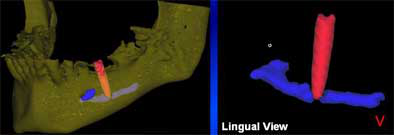
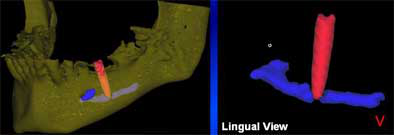
At least three vendors of dental implant reconstruction software had booths at the AAOMS meeting, Bradrick said, and all of the programs seem to operate similarly. These applications allow the oral surgeon to simulate and draw in the alveolar canal, "inserting" implants to evaluate their relation to the canal, and measure the distance between the implant and the inferior alveolar nerve (IAN) that must remain intact.
Two recent dental implant cases resulted from the use of a published but ill-conceived anesthetic technique for dental implant surgery, Bradrick said.
"To put in a mandibular implant, some surgeons aren't using the traditional inferior alveolar nerve block. Surgeons are just infiltrating the area of implant placement with local anesthetic," he said, describing the primitive technique. "Supposedly when you're getting close to an unanesthetized inferior alveolar nerve, the patient will complain of pain and you stop."
But the pain warning didn't work in two recent cases, resulting in violation of the inferior alveolar canal with accompanying loss of sensation in the jaw. Fortunately, he said, the damage in the second case was mostly reversed.
"This was a relatively new case, only about a day old. They took out the implant real quick, and she got about 90% of her sensation back," he said. "You can almost see the threads on that implant."
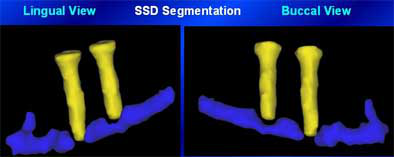 |
| Above and below: Violation of the inferior alveolar canal in two dental implant cases, seen in reconstructed CT images. The mandibular loss of sensation was reversed in the second case (below), thanks to quick removal of the implant. |
 |
Few oral and maxillofacial surgeons are actually using CT reconstruction software at this point, he said, but the techniques will certainly gain more followers as CT scanners and better software become more widely available. CT with 3D reconstructions offers significant advantages in planning for trauma surgery, cranioplasty, orthognathic surgery, dental implants, and a number of other applications.
"Conebeam office-based CT units with multiplanar and 3D reconstruction software ... are now available if you want to spend $300,000," he said.
More than a decade ago, Fishman et al showed that 3D reconstructions CT altered the management of 20% to 30% of musculoskeletal patients, concluding that surgeons prefer 3D images for planning and patient management, Bradrick said (Radiology, November 1991, Vol. 181:2, pp. 321-327). In his practice, 3D volume reconstruction software has proved to be of great value in surgical planning -- and as an educational tool for patients.
"There are so many versatile things these programs can do, you're limited only by your imagination," Bradrick said.
By
Eric BarnesAuntMinnie.com staff writer
November 22, 2004